Discovering that your child has Cerebral Palsy (CP) is a life-altering moment that brings a mountain of questions. In 2026, the medical landscape in India has evolved from merely “managing” symptoms to optimizing human potential through a blend of cutting-edge robotics, regenerative medicine, and traditional holistic care.If you are searching for the “best treatment for CP child,” it is crucial to understand that there is no “miracle cure.” Instead, there is a highly effective multidisciplinary strategy that can help your child lead a life of dignity and independence.
1. The 2026 Philosophy: From Disability to Ability – How the Best Treatment for CP Child Begins with Neuroplasticity
In 2026, we categorize CP not just by physical limitations, but by Functional Potential. Modern medicine focuses on Neuroplasticity—the brain’s remarkable ability to “rewire” itself by forming new neural connections around damaged areas.
The Golden Window of Opportunity
- Ages 0-3: This is the most critical period. The infant brain is like clay; it learns motor patterns 10x faster than an older child’s.
- Early Detection: Using GMA (General Movements Assessment) at 3 months allows doctors to start therapy even before a formal diagnosis is visible.
- The 24-Hour Rule: Treatment isn’t just a 1-hour session; it’s about how the child sits, sleeps, and plays throughout the day.
2. The Core Pillars of Rehabilitation: Foundation of the Best Treatment for CP Child
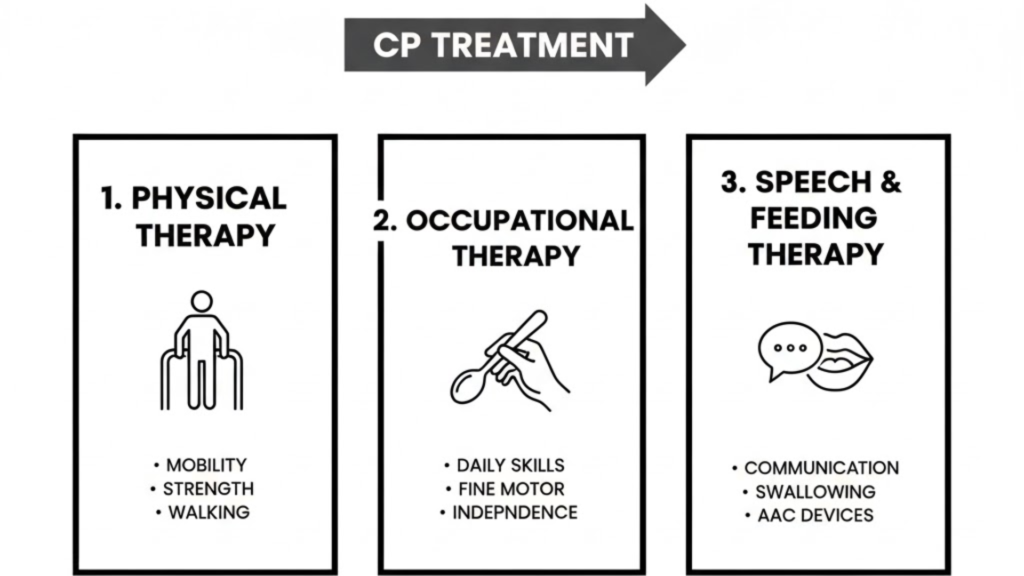
Every “best” treatment plan in India is built on these four foundational pillars.
A. Physical Therapy (PT) – Building Strength
Modern PT in 2026 has shifted toward Task-Specific Training. Instead of just stretching, we practice specific movements like standing from a chair.
- CME (Cuevas Medek Exercise): A specialized therapy that provokes automatic motor responses in children who cannot yet stand or walk.
- Hydrotherapy: Warm-water pools in major Indian cities help children move weightlessly, building muscle without the fear of falling.
B. Occupational Therapy (OT) – Building Independence
OT focuses on the “Job of Living.”
- Self-Care Skills: Teaching the child to eat, brush, and dress using adaptive tools.
- CIMT (Constraint-Induced Movement Therapy): Casting the stronger arm to force the brain to use and strengthen the weaker “CP-affected” arm.
C. Speech & Language Therapy – Building Connection
Speech therapy is about more than talking—it’s about communication and safe eating.
- Oral Motor Therapy: Strengthening jaw and tongue muscles to reduce drooling and improve swallowing.
- AAC (Augmentative Communication): Using AI-powered tablets that speak for the child through eye-tracking technology.
D. Behavioral & Cognitive Therapy
Many children with CP face comorbid conditions like ADHD or anxiety. 2026 guidelines emphasize Applied Behavior Analysis (ABA) to help manage irritability and improve school focus.
3. Comparison of Medical and Surgical Treatments: Choosing the Best Treatment for CP Child
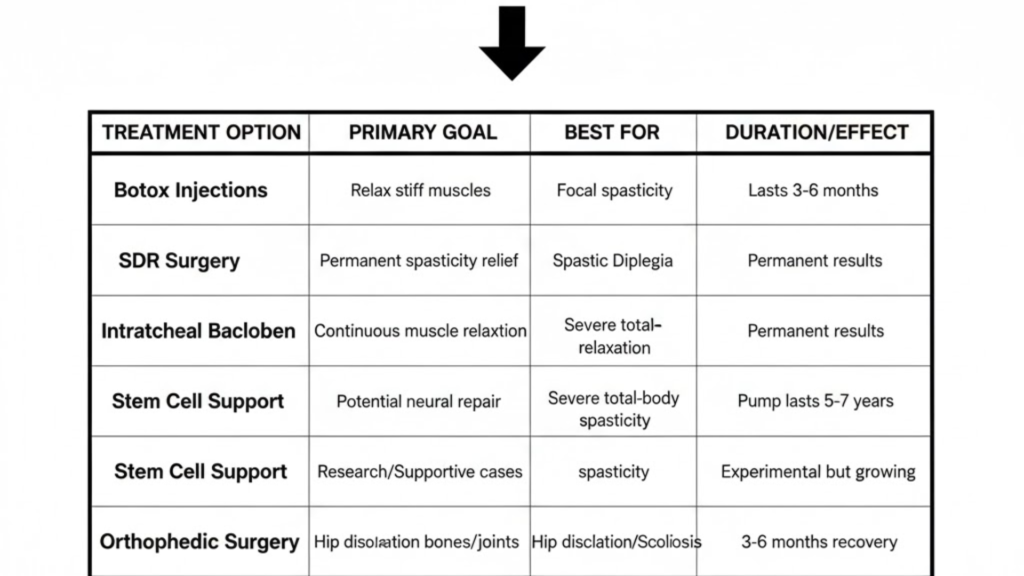
When therapies reach a plateau, medical interventions provide a “reset” for the muscles.
| Treatment Option | Purpose | Best For | Recovery / Duration |
| Botox Injections | Relax specific muscles | Focal stiffness (e.g., heel strike issues) | Lasts 3–6 months |
| SDR Surgery | Permanent spasticity relief | Spastic Diplegia (stiff legs) | 4–8 weeks recovery |
| Baclofen Pump | Continuous drug delivery | Severe, whole-body stiffness | Surgical implant |
| Stem Cell Support | Potential neural repair | Experimental / Supportive | Outpatient procedure |
| Orthopedic Surgery | Realigning bones/joints | Hip dislocation or Scoliosis | 3–6 months recovery |
4. Advanced Technology & Robotics: The 2026 Edge
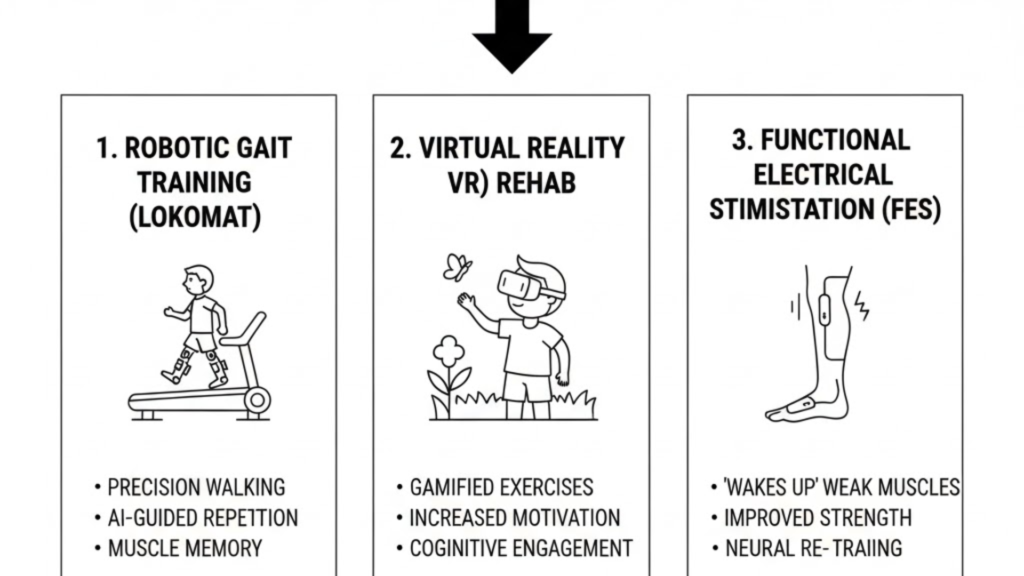
India has become a global hub for Affordable Robotic Rehabilitation. These tools provide the “intensity” that human hands cannot.
- Robotic Gait Training (Lokomat): A robotic frame that walks with the child on a treadmill, ensuring every step is perfectly aligned. This builds “muscle memory” significantly faster than traditional walking practice.
- Virtual Reality (VR) Rehab: Turning therapy into a game. A child might “fly a dragon” in VR by moving their arms, making 45 minutes of exercise feel like 5 minutes of play.
- Exoskeletons: Lightweight wearable suits that help children with severe mobility issues stand and interact with peers at eye level.
5. The Indian Holistic Advantage
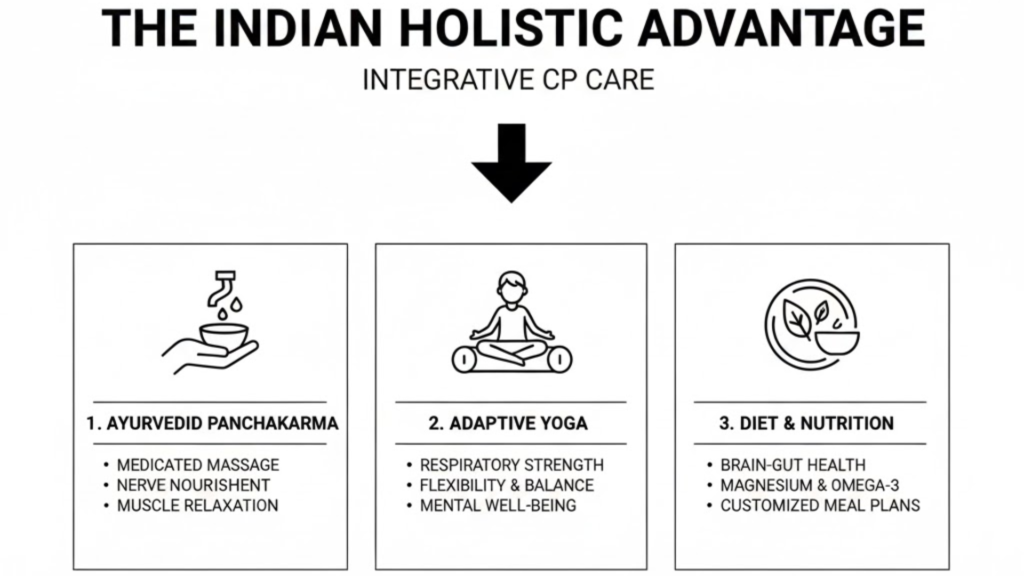
One of the reasons India is a destination for CP care is the integration of Ayurveda and Yoga.
- Ayurvedic Panchakarma: Treatments like Abhyanga (medicated oil massage) and Pinda Sweda (heat therapy with rice boluses) are excellent for nourishing weak muscles and improving blood circulation.
- Adaptive Yoga: Specialized Asanas help improve respiratory capacity (breathing) and core stability. It also provides the child with mental calm and improved sleep.
6. Education: The Right to Learn (NEP 2020)
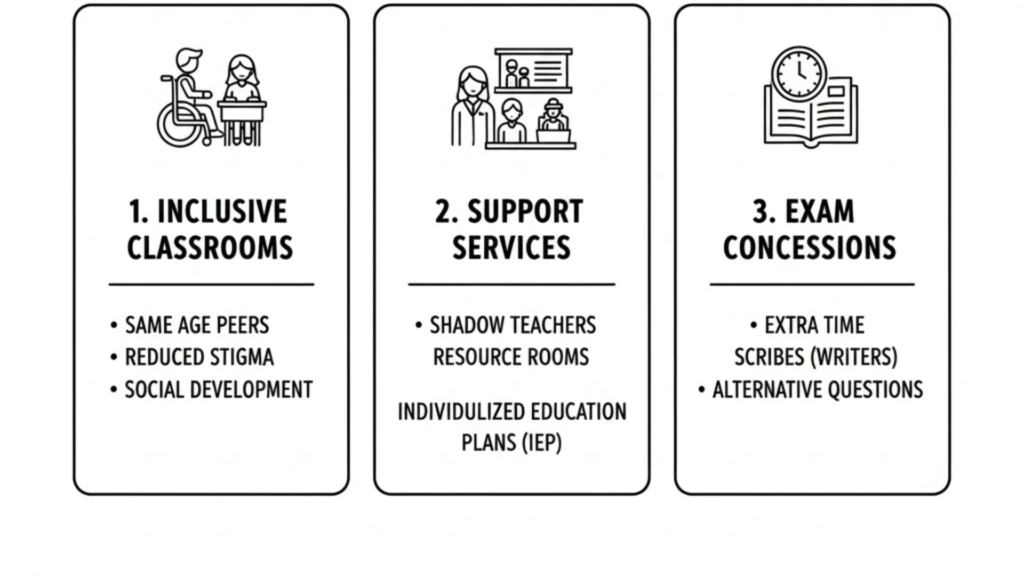
Under the National Education Policy (NEP) 2020, fully implemented by 2026:
- Inclusive Schools: Every regular school is mandated to provide admission to CP children.
- PRASHAST 2.0 App: Schools use this for early screening and to provide Resource Rooms and Shadow Teachers.
- Exam Concessions: CP children get extra time, scribes, and flexible subject choices in board exams.
7. Financial Support & Government Schemes (Expanded)
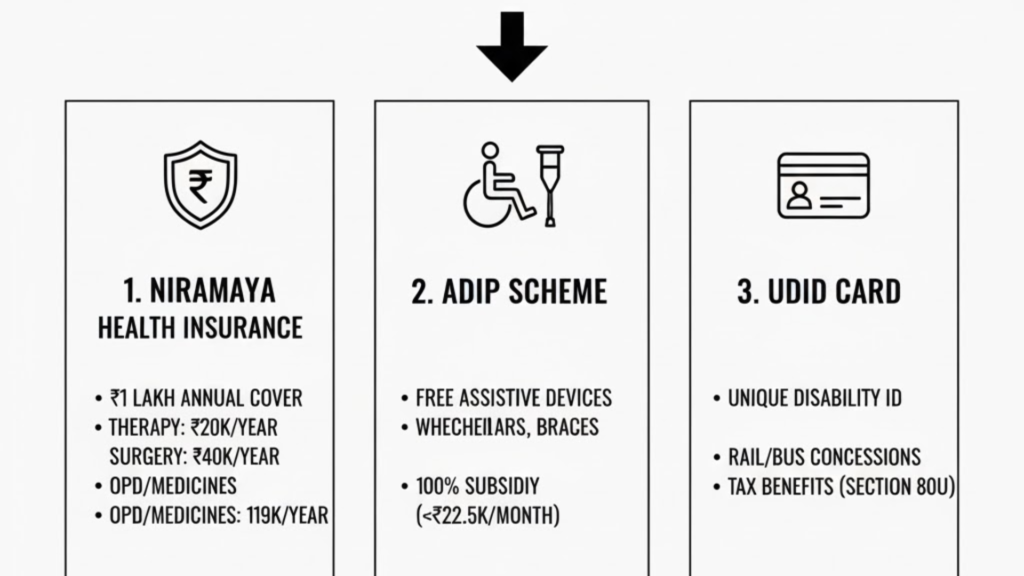
The financial burden of CP can be heavy. In 2026, the Indian government provides several “Safety Nets” that every parent must utilize to make treatment sustainable.
A. NIRAMAYA Health Insurance (The Essential Cover)
The Niramaya Scheme by the National Trust is specifically designed for CP, Autism, and Intellectual Disabilities. It offers an annual cover of ₹1,00,000 for a very low premium.
- Therapy Allowance: Up to ₹20,000 per year specifically for Physiotherapy, OT, and Speech therapy.
- OPD & Medicines: Up to ₹19,000 for routine doctor visits and diagnostic tests.
- Corrective Surgeries: Capped at ₹40,000 for surgeries that fix bone or muscle issues.
- Alternative Medicine: Up to ₹4,000 for AYUSH (Ayurveda/Yoga) treatments.
- Transportation: Provides ₹2,000 annually for travel to clinics.
B. ADIP Scheme (Free Assistive Devices)
The “Assistance to Disabled Persons” scheme provides free or highly subsidized high-quality equipment.
- Available Items: CP Chairs, high-end wheelchairs, walking frames, AFOs (braces), and customized TLM (Teaching Learning Material) kits.
- Subsidy Rules: If family income is below ₹22,500/month, aids are 100% free. For income up to ₹30,000/month, they are 50% subsidized.
C. UDID Card (The Universal Key)
The Unique Disability ID (UDID) is your child’s most important document.
- Benefit 1: Eliminates the need to carry physical medical files everywhere.
- Benefit 2: Grants 50%–75% concessions on Indian Railways and state-run bus services.
- Benefit 3: Essential for claiming Section 80U Tax Deductions (up to ₹1.25 Lakh) for caregivers.
8. Creating a “Therapy-Ready” Home (Deep Dive)
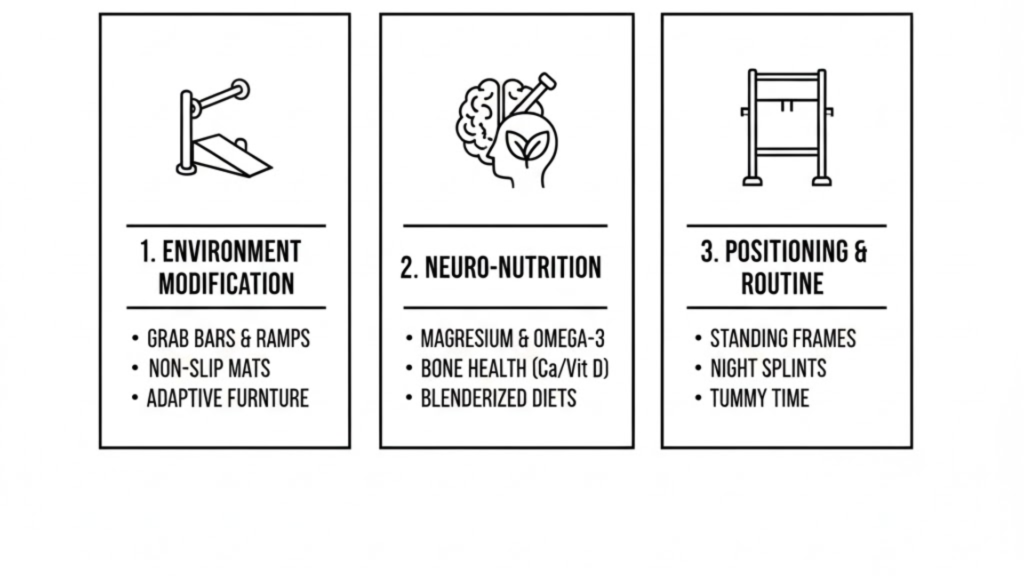
The “Best Treatment” happens in the 23 hours your child is at home, not just the 1 hour at the clinic. Your home must be turned into an Enabling Environment.
A. Environment Modification
Independence starts with a “Barrier-Free” home.
- Bathroom Safety: Install Grab Bars near the toilet and shower. Use Non-slip silicone mats to prevent falls during baths.
- Adaptive Furniture: Use a Corner Chair for floor play; it supports the back and prevents the child from slumping.
- Visual Aids: Place picture cards on drawers (e.g., a picture of a shirt on the clothes drawer) to help children with cognitive or communication delays.
B. Neuro-Nutrition: Fueling the Brain & Gut
CP children often struggle with constipation and nutrient absorption.
- Bone Health: Because CP children are at high risk for low bone density, focus on Calcium (dairy, ragi) and Vitamin D (sunlight/supplements).
- Muscle Relaxation: Magnesium (found in spinach, pumpkin seeds, and almonds) acts as a natural muscle relaxant.
- Brain Support: Omega-3 fatty acids (walnuts, flaxseeds) are crucial for nerve health.
- The “Blenderized” Diet: If your child has swallowing issues, work with a dietitian to create high-calorie, nutrient-dense purees instead of just thin liquids.
C. Positioning & Daily Routine
- Standing Frames: Using a standing frame for 45–60 minutes daily is vital. It improves hip bone development and prevents kidney stones.
- Sleep Hygiene: Use Night Splints or pillows between the knees to maintain hip alignment while sleeping.
- Tummy Time: Even for older children, supervised tummy time helps strengthen neck and back muscles.
Frequently Asked Questions (FAQ)
Q1: Can CP be cured by 2026? A: There is no “cure” that makes the brain damage disappear. However, with modern treatments, the functional impact can be reduced significantly, allowing many children to lead independent lives.
Q2: Is Stem Cell Therapy worth the cost? A: In 2026, it is considered supportive. It may improve alertness or mild motor skills, but it cannot replace intensive physiotherapy.
Q3: How do I manage my child’s drooling? A: This is often a muscle-tone issue. Speech therapy focuses on “Oral Motor” exercises. In some cases, Botox injections in the salivary glands can help.
Q4: Will my child be able to work as an adult? A: Yes! With the rise of Assistive Technology and government quotas (4% in govt jobs), many individuals with CP are successful engineers, lawyers, and artists.
Conclusion: The Roadmap to Success
The “best treatment for CP child“ in 2026 is a journey of Consistency and Hope. It requires a blend of Early Intervention, Financial Planning, and Home-Based Love. Your child’s potential is not limited by their diagnosis, but by the opportunities you provide.
